There’s a new kid on the block helping make keto easier than ever before. Newly launched, Keto Kind is a tasty plant-based keto shake that supports your ketogenic lifestyle.
Whether you are following a ketogenic diet for weight loss, managing a chronic illness, or simply improving your quality of life, Keto Kind helps make keto simple.
“Regimented health protocols can be challenging to adhere to, especially when it’s new for us. That’s why we decided to create a complete shake with 280 calories and a 3:1 keto ratio* to help make keto easy, and to provide an alternative for those who work in offices, have long commutes, can’t cook, or don’t have access to high-quality snacks.” — Andres, Co-Founder.
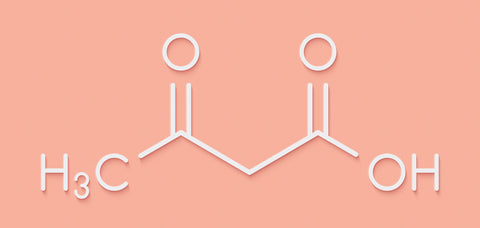
*Ketogenic ratio as in having more than 75% of its calories coming from a fat source
The best part is Keto Kind is backed by science!
Made from minimal high-quality ingredients, Keto Kind is a whole food based nutritional shake to complement your low carb meals while staying in ketosis. Our shakes are made from healthy fats like medium-chain triglycerides (MCTs) from coconuts and avocado oil, a moderate amount of protein from pea, and no sugar! Our shakes come in two delicious flavors: Vanilla Bean and Cacao. At the same time, Keto Kind contains no artificial flavorings or sweeteners, additives, sugar alcohols, or vegetable/seed oils, and all of our ingredients are plant-based and certified organic.
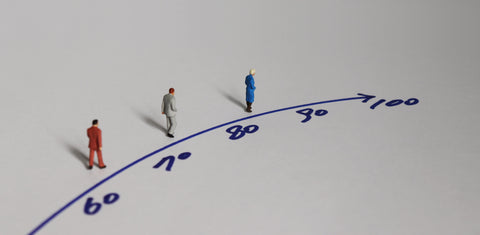
Since the 1990s, the foot has been on the gas of ketogenic research, and it doesn’t seem to be letting up. Every day there seems to be a new study published touting the benefits and therapeutic potential of keto for everything from diabetes and weight loss to Alzheimer’s disease and cancer. Unfortunately, the more the ketogenic diet is popularized by big media, the more baggage it seems to carry. Many companies have followed the hype, releasing products using ingredients and marketing tactics that confuse even the most astute consumers.
Keto Kind has nothing to hide; it was formulated under the scrutiny of the world’s leading ketogenic doctors, scientists, and practitioners to deliver a clinical-grade nutritional shake for anyone following a low carb or ketogenic diet. You can rest assured knowing Keto Kind is backed by some of the leading voices in keto, such as our Chief Medical Officer, Dr. Nasha Winters, a licensed Naturopathic Doctor, Miriam Kalamian, EdM, MS, CNS, Keith Baar, PhD, and several other world-renowned experts in the space. See our Scientific Advisory Board to learn more about our awesome team!
Everyone, including patients using a ketogenic therapy, deserve access to high-quality nutrition.
One of our missions is to make keto more accessible and enjoyable for patients using a ketogenic diet as a metabolic therapy, so we’ve made sure that Keto Kind fits even the strictest clinical guidelines for ketosis, providing patients and practitioners with a ketogenic product they can trust!
We are taking a stance against the inadequate nutritional support provided to patients managing chronic conditions. The current “nutritional” shakes offered to patients are loaded with sugar and have no place in health care. Replacing these with a low-sugar option like Keto Kind could make a huge difference in how patients respond to and recover from treatments across the board. Our long-term goal is for Keto Kind to be readily available in hospital settings to provide patients with better alternatives.
Kindness is important to us.
At Keto Kind, we want to provide a caring human touch to our customers and patients. To us, this means cultivating community, building strong relationships with our consumers, and maintaining transparency so you feel safe and confident in what Keto Kind can offer you. We want to make a difference in the lives of those that might not have ready access to quality nutrition, which is why we will be donating product to low-income hospitals for use in metabolic therapies.
The people behind Keto Kind.
Keto Kind’s founders, Andres and Mauricio, are two undergraduates, young scientists, and best friends since kindergarten. Together, they were empowered by the potential of keto when Mauricio used it to reverse his pre-diabetes. After sharing the benefits they experienced with their families and seeing their health improve, they knew keto was more than just a fad diet. Andres and Mauricio made Keto Kind for anyone out there struggling to adhere to the diet (like they did) and provide a nutritious option to patients undergoing metabolic therapies.
Written by Kristi Storoschuk in collaboration with Keto Kind